By:
Published: August, 2023
How have social insurance and related programs improved – or exacerbated – inequality during the COVID-19 pandemic? What policy adjustments affected inequality, for better or worse?
Health, Health Insurance, and Health Care
COVID-19 and Nursing Facilities
Mortality due to COVID-19 disproportionately affected nursing home residents. Medicare beneficiaries in nursing homes were 14 times more likely to be diagnosed with COVID-19 than beneficiaries living in the community (independent of the age of the individual).
- Black nursing home residents were more likely to live in facilities with low vaccination rates of both staff and residents. Those facilities were also more likely to be for-profit, dependent on Medicaid financing, and to receive low ratings by CMS standards.
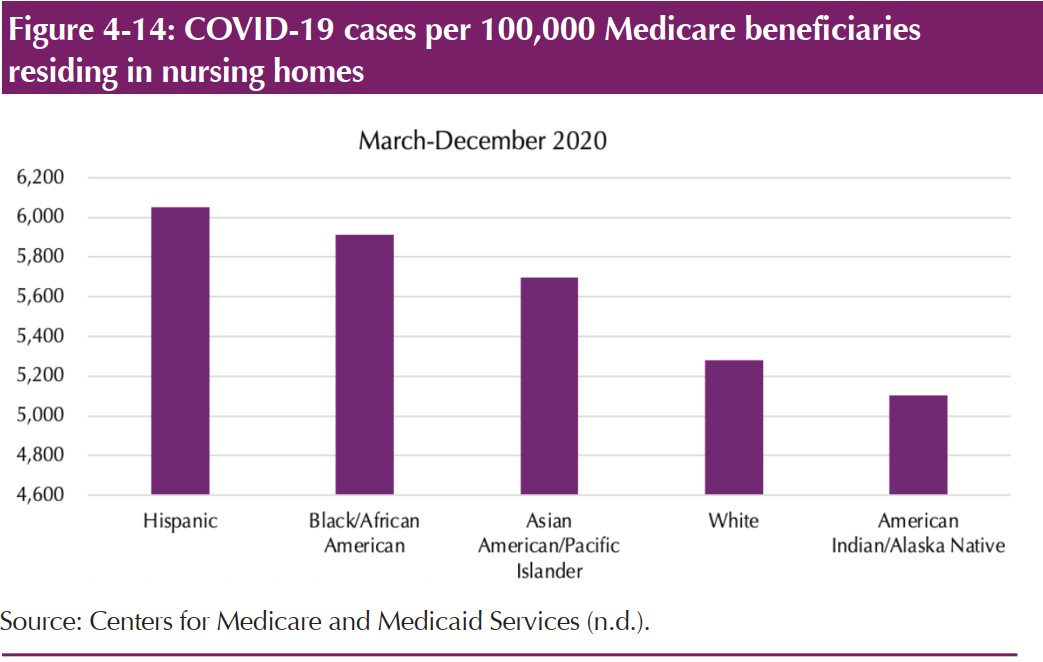
- Black, Hispanic, and American Indian / Alaskan Native Medicare beneficiaries in nursing homes had markedly higher rates of cases of COVID-19 than White or Asian / Pacific Islander beneficiaries.
Medicaid and the ACA Marketplaces
Congress increased the share of Medicaid and the Children’s Health Insurance Program (CHIP) spending financed by the federal government. Rates of uninsurance fell sharply across the income spectrum during the pandemic, with the sharpest decline among families with incomes between 100 to 199% of the poverty line.
- Rates of uninsurance fell for all racial / ethnic groups, with the exception of American Indian / Alaskan Natives – the group with the highest rate of uninsurance overall.
- Continuing the ability to remain enrolled in Medicaid / CHIP for 12 months regardless of income changes could help mitigate racial disparities in uninsurance rates, since Black, Hispanic, and American Indian / Alaskan Native individuals have lower overall rates of coverage than White individuals.
Telemedicine
The use of telemedicine expanded during the pandemic, but did not increase sufficiently to offset the impact of the drop in in-person health care services. Access to telemedicine services was not distributed equally across populations.
- Low-income, elderly, and non-White individuals have less access to and/or comfort with digital services and computers.
- Black and elderly adults were less likely to use video telehealth services.
- Audio-only telemedicine services partially, but not entirely, offset disparities in access to telemedicine services amongst Medicare beneficiaries by sex, income, and location.
The Provider Relief Fund
The pandemic threatened the financial stability of many health care providers, especially “safety net” providers that serve disproportionately uninsured individuals or patients with Medicaid. The Provider Relief Fund delivered relief funds to providers quickly, but not efficiently.
- Providers with more dependence on commercial insurance companies received larger relief grants than those more dependent on Medicare and Medicaid. Thus, funds were disproportionately given to the least financially stressed providers.
- This relief fund exacerbated, rather than improved, health care access disparities for Black, Hispanic, and American Indian / Alaska Native patients.
Income Security
Unemployment Insurance (UI)
Congress made changes to the UI program during the pandemic that dramatically, but temporarily, expanded eligibility, the benefit amount, and the duration of benefits.
- Overall, lower-wage workers benefited more from the pandemic expansion in UI benefits than higher-wage workers.
- Black and Hispanic unemployed workers were less likely to receive UI benefits than White unemployed workers.
Child Tax Credit (CTC)
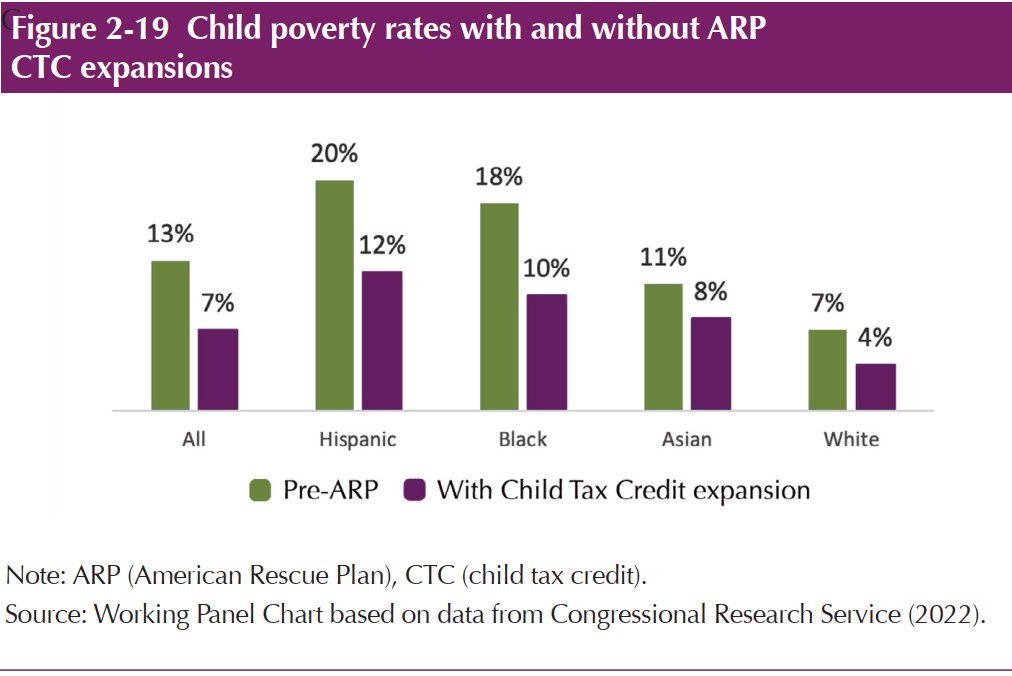
Temporary changes to the CTC under the American Rescue Plan increased the maximum credit amount for lower-income families and made the credit fully refundable, meaning lower-income families would receive the entire amount of the credit.
- If maintained, the expanded CTC would lower child poverty rates by nearly 50%
- Black and Hispanic households with children would see the largest declines in poverty.
The combined effects of the expansion of UI, the CTC, and the Economic Impact Payments resulted in a sharp overall drop in childhood poverty
Food Assistance
Supplemental Nutrition Assistance Program (SNAP)
Congress progressively expanded SNAP during the public health emergency by: offering flexibility to states to simplify the application and recertification processes; providing financial support for administering the program; and increasing the baseline for benefit amounts.
- These changes led to an overall 16% increase in enrollment in 2020, which remained still 12% higher than pre-pandemic levels as of March 2022.
- Since SNAP benefit amounts are tied to income, White beneficiaries – who generally have higher incomes – received a bigger increase in benefits (95% increase) than Black (84%) and Hispanic (78%) beneficiaries.
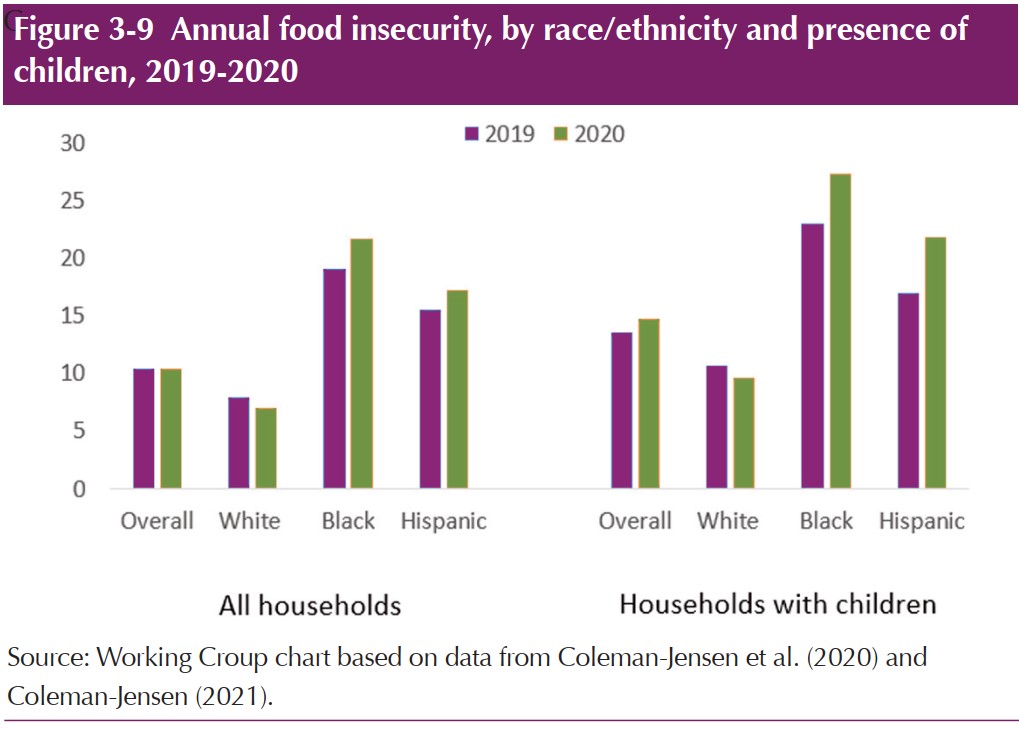
Overall, the pandemic exacerbated racial and ethnic disparities in food security; the rate of food insecurity declined for White families, but increased for Black and Hispanic families.
dddddddddddddddddd